How to Read an EKG: A Comprehensive Guide for Modern Healthcare in 2025
Understanding how to read an EKG (electrocardiogram) is an essential skill for healthcare professionals. This guide aims to demystify EKG interpretation for modern practitioners, with a focus on recognizing common patterns, understanding EKG waves, and applying techniques in clinical practices. Here, you’ll find practical tips on how to effectively analyze EKG results and enhance patient care.
Understanding EKG Waves
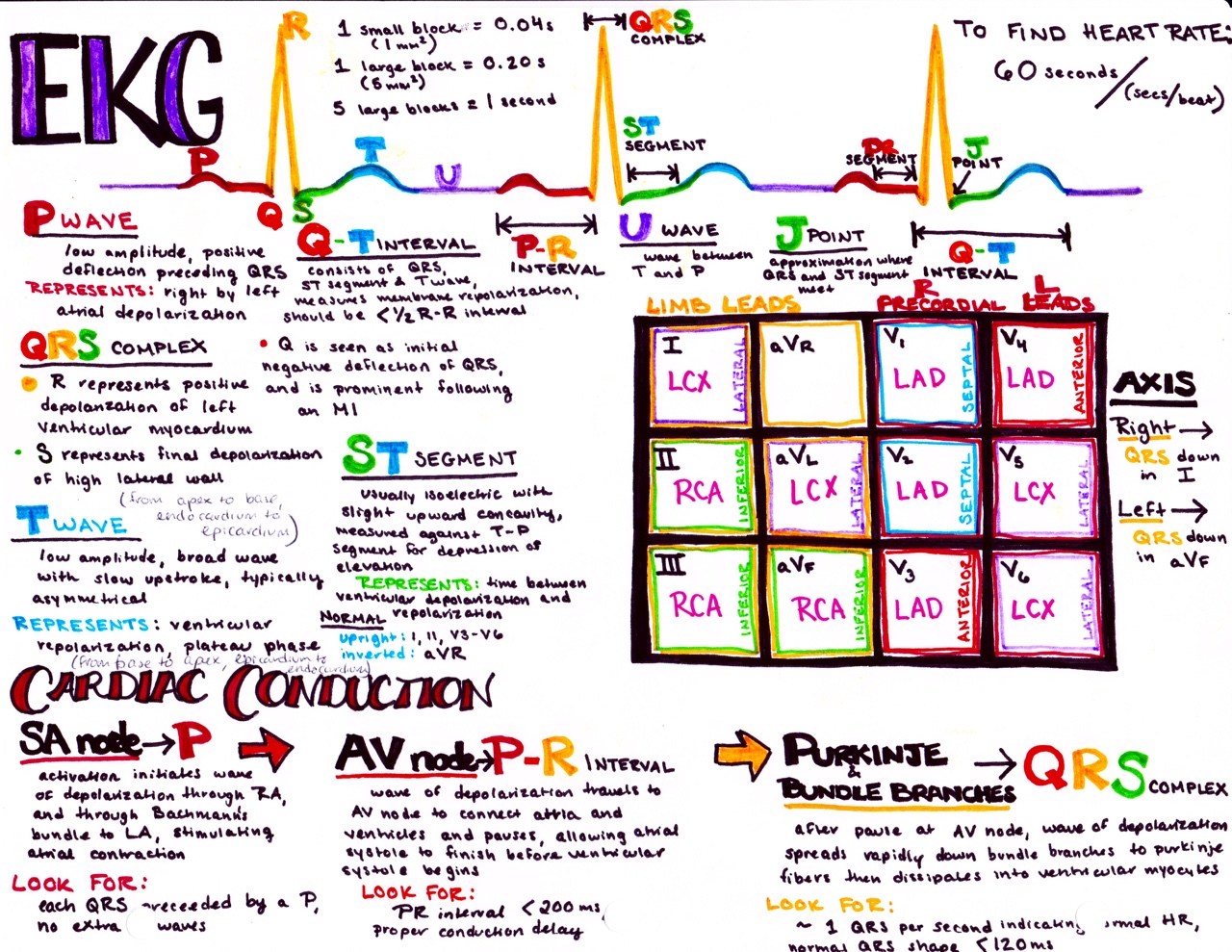
Deep comprehension of the **understanding EKG waves** is critical for accurate interpretation. The EKG waveform comprises several components: the P wave, QRS complex, and T wave, each representing different physiological activities of the heart. The P wave indicates atrial depolarization; meanwhile, the QRS complex signifies ventricular depolarization, and the T wave represents ventricular repolarization. Understanding these elements facilitates **interpreting EKG results**, focusing on the sequence and significance of these waves.
P Wave Analysis
The P wave is one of the first visual indicators on an EKG strip. When learning how to read an EKG, it’s essential to recognize its morphology and duration. A normally shaped P wave indicates healthy atrial activity. If the P wave is absent or significantly altered, this may signify underlying issues such as atrial fibrillation. Special attention should also be paid to the intervals between the P wave and the QRS complex to assess for conditions like **conduction delays**.
QRS Complex Interpretation
The QRS complex represents ventricular depolarization and is much larger than the P wave in amplitude. When analyzing how to read an EKG, examine the width and morphology of the QRS complex. A **prolonged QRS** can indicate conditions like **bundle branch block** or ventricular hypertrophy, while an abnormally shaped QRS may suggest myocardial infarction. Understanding and recognizing these potential **EKG abnormalities** is crucial in patient assessment.
T Wave Significance
The T wave follows the QRS complex and generally indicates the heart’s recovery period or repolarization. Monitoring T wave abnormalities can signal a variety of problems—it can point to electrolyte imbalances or ischemic changes when inverted. A flat or peaked T wave could also indicate potential cardiovascular issues, making the evaluation of T waves an integral part of **heart rhythm analysis**.
Common EKG Patterns
Familiarizing yourself with **common EKG patterns** can enhance the efficacy of patient monitoring. Certain patterns are signatures of specific heart conditions, making their recognition critical in **clinical guidelines**. The most common ECG patterns to look for include normal sinus rhythm, atrial fibrillation, and ventricular tachycardia, among others.
Normal Sinus Rhythm
Normal sinus rhythm is characterized by the regular rhythm of the heart, with P waves followed by a QRS complex consistently displayed at a regular interval. This pattern usually ranges between 60-100 beats per minute. Understanding this is a fundamental aspect of cardiology basics and can serve as the baseline when assessing patients for **cardiac arrhythmias** or other **cardiovascular diseases**.
Atrial Fibrillation
Atrial fibrillation is another common and significant finding you may encounter while interpreting EKG results. It manifests as an irregularly irregular rhythm with no distinct P waves. Instead, you will observe irregular ventricular responses. Recognizing atrial fibrillation quickly is vital for effective treatment and **nursing responsibilities**, as this condition elevates the risk of stroke if not managed correctly.
Ventricular Tachycardia
The identification of ventricular tachycardia (VT) is crucial and can be recognized by aSequence of rapid QRS complexes, typically 3 or more in a row, with a broad shape. VT requires urgent attention due to its potential to evolve into more serious conditions like ventricular fibrillation. The clinical knowledge surrounding this pattern is a valuable asset that can assist in identifying heart conditions promptly.
Advanced EKG Concepts
Advanced concepts in how to read an EKG critically involve understanding **EKG lead placement** and the technology used in EKG readings. Knowledge of these aspects can provide deeper insight into the patient’s cardiac health.
EKG Lead Placement
Correct lead placement is essential for accurate readings, providing appropriate visualization of the electrical activity of the heart. The 12-lead EKG is the most commonly used configuration, which includes limb and precordial leads. Improper lead placement can result in misinterpretation of EKG data, making knowledge of proper techniques necessary for effective cardiac monitoring and **health screening**.
Utilizing EKG Equipment
Modern technology also plays a key role in EKG analysis. Advanced **EKG equipment** and wearable **EKG devices** offer critical assistance in acute care settings. Familiarity with such devices not only enables effective data collection but also enhances patient engagement and education. These technologies are pivotal in evolving **telemedicine applications**, allowing practitioners to monitor patients remotely and more efficiently.
Cardiology Techniques for Patient Assessement
Understanding various cardiology techniques, including stress testing and echocardiography, can complement EKG interpretation effectively. Integrating multiple methods will enhance clinical decision-making and improve risk assessments, leading to better patient outcomes. Continuous education through **medical certification courses** will augment these skills further.
Conclusion
Understanding how to read an EKG is a fundamental skill that combines knowledge of cardiac anatomy, physiology, and applications of technology. An emphasis on practical and efficient EKG interpretation not only highlights potential heart-related issues but also fosters better **patient care** and makes healthcare providers more effective in their roles. Proper training and a solid foundation in cardiology raise the bar for clinical practices in 2025 and beyond.
FAQ
1. What are common EKG abnormalities to watch for?
Common EKG abnormalities may include atrial fibrillation, ventricular tachycardia, and ST elevation, which could indicate conditions like myocardial infarction. Regular training and engagement in an **EKG interpretation course** can help professionals stay informed about these signs for effective patient assessment.
2. How does EKG lead placement affect outcomes?
Improper EKG lead placement can lead to distorted representations of the heart’s electrical activity, resulting in misdiagnosis. Adequate training in **lead configurations** is fundamental to accurate **cardiac monitoring processes**, ensuring no discrepancies in patient data.
3. Why is EKG interpretation important in critical care?
In **critical care**, EKG interpretation is paramount as it aids in real-time decision-making regarding cardiac status. Recognizing lifelines like arrhythmias swiftly allows healthcare providers to initiate timely treatment, which can be **life-saving skills** in a patient’s journey.
4. Can wearable EKG devices aid in early detection?
Yes, wearable EKG devices can significantly contribute to early detection of heart conditions by allowing continuous monitoring and immediate feedback systems. Utilizing these devices promotes active engagement with health, allowing for proactive management of cardiovascular health.
5. What background is needed for effective EKG reading?
A strong foundation in medical education, especially **cardiology basics**, is essential for effective EKG reading. Understanding cardiac anatomy, physiology, and rhythm analysis alongside practical experience can significantly enhance a healthcare professional’s competency in interpreting EKG results accurately.
6. What is the role of EKG in patient care techniques?
EKG plays a vital role in patient care techniques, particularly as it identifies arrhythmias, ischemic changes, and other cardiac anomalies quickly. This information enables healthcare professionals to tailor treatment plans effectively, improving patient outcomes.