Understanding Insulin Syringes and Dosages
How Many Units in an Insulin Syringe?
When it comes to managing diabetes effectively, understanding insulin syringes is crucial. Typically, **1 ml** in an insulin syringe equates to **100 units of insulin**. This means each unit corresponds to **0.01 ml**, making it essential for individuals to accurately measure their insulin dosage. By using the correct markings on the syringe, patients can ensure precise insulin delivery. However, variations in syringe designs might exist, so always confirm the measurements printed on your specific syringe to avoid miscalculations.
Insulin Syringe Marking System
The **insulin syringe marking system** is vital for **accurate insulin dosing**. Generally, syringes are marked to help users measure their dosages effectively. Each unit is represented clearly on the body of the syringe, allowing for straightforward tracking of the **insulin dosage** to be administered. Users must familiarize themselves with this marking system, as even minor miscalculations can lead to significant fluctuations in blood glucose levels. Following **healthcare guidelines for insulin** can further enhance diabetes management and promote safe insulin usage across various injection sites.
Measuring Insulin Accurately
For effective diabetes management, knowing how to measure **insulin accurately** is essential. To achieve precision, draw air into the syringe before extracting insulin, as this helps facilitate a smoother transition from the vial. Ensure that there are no bubbles in your syringe as these can alter the dosage. By following this **insulin delivery method**, diabetes patients can enhance their daily insulin intake accuracy, which is fundamental for maintaining stable blood sugar levels.
Insulin Dose Calculation for Patients
When calculating insulin doses, many factors come into play, including activity level, carbohydrate intake, and current blood sugar readings. Tools such as food diaries and **blood sugar testing** can aid in determining the appropriate **insulin dosage**. Healthcare providers often recommend adjustments to dosages to best fit the patient’s lifestyle, thus enhancing overall diabetes care. Additionally, utilizing an **insulin pump** can simplify dosage calculations, effectively corresponding insulin delivery with real-time needs.
Conversion of ml to Units in Insulin Syringes
Understanding the **conversion of ml to units** is crucial for anyone using insulin syringes. As a general rule, **1 ml is equal to 100 units of insulin**, which translates to **10 units of insulin per 0.1 ml**. It’s vital to recognize this conversion when preparing insulin doses, particularly for those on varying insulin treatments. Regularly reviewing **insulin syringe capacity** and markings ensures that individuals maintain optimal control over their insulin therapy.
Best Practices for Insulin Injections
Executing the right technique during insulin injections can greatly influence treatment outcomes. Always select an appropriate injection site—common locations include the abdomen, thighs, and upper arms. Rotate injection sites to minimize potential complications and **injection site problems**. Practicing **proper insulin injection techniques** not only reduces discomfort but also helps prevent insulin absorption inconsistencies, crucial for blood sugar management.
Understanding Insulin Dosage Adjustments
It’s important to monitor blood sugar levels frequently to determine whether insulin dosage adjustments are necessary. Many diabetic patients must tweak their insulin requirements based on **lifestyle changes** or changes in **blood sugar testing** results. Consult with healthcare providers for **insulin dosage adjustments** to ensure that diabetes management is personalized and responsive to individual patient needs. Utilizing community resources for diabetes can also help reinforce good habits.
Common Insulin Dosing Mistakes
**Common insulin dosing mistakes** can lead to serious health complications. One issue often encountered is misjudging the volume of insulin injected due to improper readings on the syringe. To combat this, always double-check measurements and confirm with a healthcare professional when uncertain. Educating patients about routines for verifying dosages can bolster **insulin therapy education**, promoting lift in compliance rates and overall effectiveness of diabetes management plans.
Insulin Delivery Methods and Safety
Using the correct **insulin delivery methods** is essential in managing diabetes. Insulin syringes remain one of the most common tools; however, innovations such as **insulin pens** and **insulin pumps** offer alternative methods that some patients may find more convenient for daily use. While each method of insulin delivery has advantages, ensuring safety protocols and **insulin storage guidelines** are followed will help manage diabetic treatment regimens effectively.
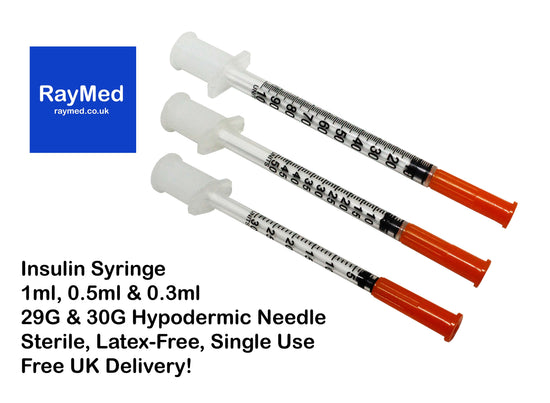
Advantages of Insulin Syringes
Despite the advancements in insulin delivery technology, there are several notable **advantages of insulin syringes**. For example, they allow for greater flexibility in dosing and enable patients to draw different types of insulin as needed. Additionally, syringes were established as one of the most reliable methods in managing **insulin therapy**. Coupled with the advantage of **syringe volume measurement**, patients can administer precise doses tailored to their needs, enhancing their overall insulin management experience.
Best Practices for Insulin Storage
**Proper insulin storage** is critical for maintaining the efficacy of the medication. Insulin should be stored in a cool, dry place, away from direct sunlight. Never store insulin in extreme temperatures, as this can adversely affect its potency. Familiarizing yourself with **insulin storage guidelines** and periodically checking expiration dates helps ensure that the medication remains effective and safe for use.
Emergency Use of Insulin and Patient Education
Understanding how and when to use insulin in emergencies is a vital aspect of diabetes care. Having a plan for common insulin emergencies can also alleviate the impact of unexpected blood sugar fluctuations. **Patient education on insulin** should encompass recognition of signs of hypoglycemia and the correct methods of treatment, which may include using glucose tablets or administering a quick-acting insulin dosage.
Key Takeaways
- Each ml in an insulin syringe typically corresponds to 100 units of insulin.
- Accurate measurement and understanding of the insulin syringe marking system are essential for effective diabetes management.
- Proper techniques in insulin injections can mitigate discomfort and improve insulin absorption.
- Awareness of dosage adjustments based on lifestyle changes and frequent testing is crucial for optimal insulin therapy.
- Emergency preparedness plays a significant role in insulin safety and effective patient care.
FAQ
1. What is the difference between an insulin syringe and an insulin pen?
Insulin syringes and insulin pens are both tools used for insulin delivery but differ in design and usability. **Insulin pens** are prefilled devices allowing for more convenient, portable administration, while syringes require drawing insulin from a vial. Each method has distinct advantages, and patients may choose based on comfort and lifestyle needs.
2. How do I avoid common mistakes when using an insulin syringe?
To avoid errors while using an insulin syringe, double-check the measurement before the injection. Ensure your hands are clean and the needle is sharp and sterile. Practice rotating injection sites to minimize pain and ensure consistent absorption. Following these steps can prevent common pitfalls and support effective diabetes care.
3. Can I reuse insulin syringes?
Reusing insulin syringes is generally not recommended due to the risk of infection and decreased effectiveness. Each syringe is designed for single-use, maintaining safety in insulin delivery practices. Dispose of used syringes properly according to local disposal guidelines to avoid injury or contamination.
4. How should I store opened insulin vials?
Opened insulin vials should be stored in the refrigerator and used within a specified period, usually up to 30 days, depending on the type of insulin. Avoid freezing or exposing the insulin to excessive heat or light, which could reduce its effectiveness over time.
5. What should I do if I experience low blood sugar after an insulin injection?
If you experience low blood sugar symptoms, such as sweating, trembling, or confusion, immediately consume fast-acting carbohydrates like glucose tablets, juice, or candy. Follow up with a protein snack to sustain blood sugar levels. If severe symptoms persist, seek medical assistance promptly.